Convalescent plasma is safe to treat COVID-19: nationwide study
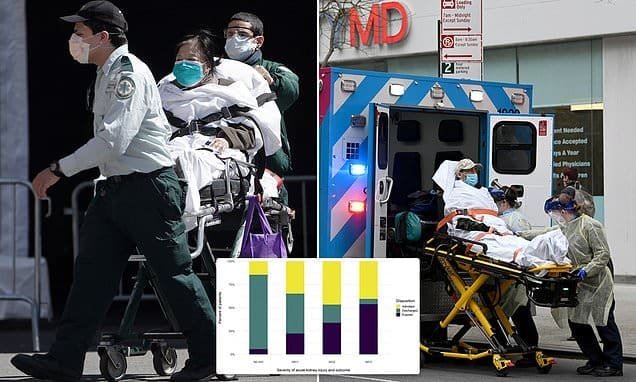
The most comprehensive national study to date has found that convalescent plasma appears to be safe to use on COVID-19 patients, a promising development in the race to find a treatment for the deadly virus. But the study didn’t determine whether the treatment works.
A team of more than 5,000 doctors from over 2,000 hospitals and laboratories have been testing the experimental therapy, which involves transfusing the antibody-rich blood serum of recovered COVID-19 patients into people who are battling the illness.
Of the 5,000 seriously ill patients who received blood plasma transfusions for the study, fewer than 1 percent experienced serious adverse events. The mortality rate seven days after treatment was 14.9 percent, but the researchers noted the infusion patients were already gravely ill and the rate “does not appear excessive.”
“We’re very encouraged that the treatment is safe,” Dr. Michael Joyner, a physiologist at the Mayo Clinic and the principal investigator of the study, told NBC News. “That was really the first hurdle for us. And showing that it’s safe gives us confidence to move on and begin to try to understand the efficacy.”

The study, which was co-authored by researchers at several institutions including Michigan State University and Johns Hopkins, hasn’t undergone peer review or publication in a scientific journal. The results were posted on a public server, called MedRxiv, so that other scientists and physicians could quickly review the data.
“I’ve never put a paper on a preprint server before in my life, and I’ve published almost 500 papers,” Joyner said. “We wanted to get them out there to the treating physicians and the general public as soon as we could.”
Joyner said the researchers will start receiving data on the treatment’s effectiveness in the next few weeks. He expects to have a “much clearer picture” within the next several months.
“We’re really trying to build the plane and fly it at the same time,” Joyner added. “And the fact that we’re able to get at least some analysis done so quickly, we’re very pleased with that. We hope to do more really almost in real time.”
Convalescent plasma therapy isn’t a new form of treatment. It has been used to fight past virus outbreaks, including Ebola, influenza and SARS.
But it hasn’t been used widely in the United States for decades, and its effectiveness has never been scientifically established due to a lack of robust trials.
Let our news meet your inbox. The news and stories that matters, delivered weekday mornings.
The study notes that the most common complication of convalescent plasma therapy is transfusion associated circulatory overload (or TACO), which occurs when a patient cannot tolerate the increased blood volume that results from the transfusion of plasma. Researchers were also concerned about the possibility that the antibodies infused into patients could lead to the formation of new infections.
But the 5,000 transfusions studied resulted in few such complications, the report says.
A total of nearly 10,500 COVID-19 patients have now received the treatment at facilities across the country, according to the Mayo Clinic in Rochester, Minnesota.
Doctors at Mount Sinai Hospital in New York City, which is part of the national coalition, have used it on more than 350 COVID-19 patients.
Dr. Nicole Bouvier, one of the leaders of the hospital’s plasma program, said an analysis of their first 39 patients suggests it is most effective when used in the early stages of the virus.
“It’s not a magic bullet. It doesn’t cure everybody,” she said. “But on the whole, patients who have gotten convalescent plasma have gotten better, quicker and more often, than similar patients who didn’t get convalescent plasma.”
One of those patients was Claudia Garcenot, a New York City woman who contracted COVID-19 about six weeks ago.
Garcenot is the chief nursing officer at Mount Sinai Brooklyn, a bustling hospital hit by an influx of coronavirus patients throughout the month of March.
One day near the end of the month, Garcenot felt a wave of fatigue followed by shortness of breath. Her symptoms soon worsened, prompting her to go to a hospital where she tested positive for COVID-19. A chest X-ray revealed she had bilateral pneumonia as well.
Garcenot went home to recover but her condition worsened as her breathing became more labored.
She rushed to her hospital’s emergency room.
“Of course, I heard all those horror stories about this is what happens with COVID,” Garcenot said. “You get sick. You don’t feel well. Then you get viral pneumonia and then you end up on a ventilator.”
Garcenot was eventually admitted to Mount Sinai Hospital in Manhattan because no beds were available at her hospital. A few days later, when it appeared she ran the risk of being put on a ventilator, Garcenot found out she was a candidate for convalescent plasma treatment.
As the medical team described the process, the severity of her condition set in.
“I really wasn’t a nurse at that moment,” Garcenot said. “I was a really frightened, sick patient, who was worrying about surviving.”
She received two doses of convalescent plasma April 5, a process that took four hours. Just over a day later, she woke up in the morning feeling like a different person.
“I remember taking that first deep breath,” Garcenot said. “Even though I still felt the tightness in my chest, I felt like I had oxygen.”
“I breathed in again and I thought to myself, ‘It’s got (to be) the plasma,’” she added. “I felt like I’d won the lottery.”
Some 48 hours later, with her fever gone and her oxygen levels back to normal, Garcenot was discharged from the hospital.
While researchers may not have yet come to a conclusion about the effectiveness of convalescent plasma, Claudia Garcenot has.
“I really believe that receiving that plasma treatment is what changed the course of my illness,” she said.



Recent Comments